Who could benefit from a hip replacement?
If you have substantial pain, inflammation,
and damage to your hip joint as a result of disorders like:
- Osteoarthritis (most common)
- Rheumatoid arthritis
- Avascular necrosis (osteonecrosis)
- Hip fractures or tumors in the joint.
Types of hip replacement
Your surgeon will perform a whole or partial hip
replacement:
- Total hip replacement: Involves a surgeon replacing the
whole hip with a prosthetic joint. They will replace your thighbone's top
(femoral head) and the socket it fits into (acetabulum). Most hip
replacements are complete hip replacements.
- Partial hip replacement: Partial hip replacements are
quite unusual. Your surgeon will replace only a portion of your hip. These
are often used exclusively to repair certain forms of fractured hips (hip
fractures) or to remove specific types of malignancies.
When is the time to go for a hip replacement?
When hip discomfort impairs your quality of life, it
may be time to consider hip replacement surgery. Signs of diminishing quality of
life include difficulty sleeping, difficulty accomplishing simple chores like
dressing, and limited participation in enjoyable activities.
At first, your doctor may suggest other therapies such as
pain or inflammatory medications, walking aids, joint injections, and physical
therapy. If these treatments do not alleviate the pain and stiffness, hip
replacement surgery may be required to restore function and enhance the quality
of life.
Difference Between traditional and minimally invasive hip
replacements?
Minimally invasive hip replacement.
Minimally invasive hip replacement tries to reduce the
impact of surgery on healthy tissues including muscles and blood vessels. While
anterior hip replacement has been advertised as a minimally invasive procedure,
orthopedic surgeons today employ minimally invasive procedures for all surgical
approaches to the hip. Your surgeon will explain which strategy may provide the
greatest results.
This method may offer benefits such as less muscle
damage, discomfort, faster healing, less limping, shorter hospital stay, and
reduced risk of hip dislocation.
Minimally invasive hip replacement is not suitable for many
individuals. Your age, weight, exercise level, and other characteristics will
assist the surgeon in determining whether you are a good candidate.
Traditional Hip Replacement
A classic hip replacement involves a single, wide
incision that allows the surgeon to obtain access to the hip, which is often
done from the side (lateral approach) or the back (posterior approach).
Recovery after a typical hip replacement might take a
while since the surgeon must cut through or detach several muscles and tendons
to reach the joint. (The muscles and tendons are healed while the hip implants
are in place.) You may be at risk of dislocation until all of the supporting
components in your new hip have healed.
Consult with your orthopedic hip surgeon to determine the
best surgical technique for you.
The Orthopaedic Evaluation
An assessment with an orthopedic surgeon includes various
components:
- Medical history.
- Physical exam.
- X-Rays.
- magnetic resonance imaging (MRI) scan,
What Happens in Hip Replacement -
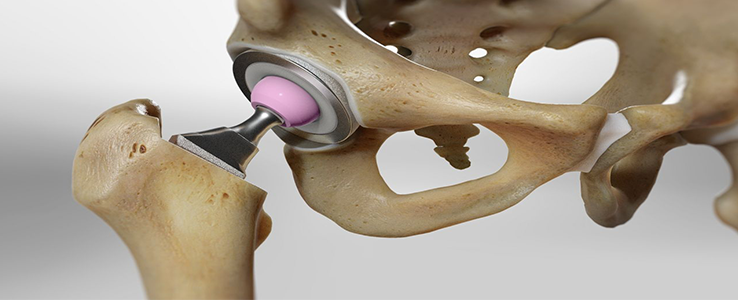
A total hip replacement (also known as total hip
arthroplasty) involves removing the diseased bone and cartilage and replacing it
with prosthetic components.
- The injured femoral head is replaced with a metal stem inserted into the
hollow middle of the femur. The femoral stem can either be cemented or
"press fit" into the bone.
- A metal or ceramic ball is inserted into the top half of the stem. This
ball replaces the injured femoral head, which was removed.
- A metal socket is used to replace the injured cartilage surface of the
acetabulum. Screws or cement are occasionally used to secure the socket in
place.
- To provide a smooth gliding surface, insert a spacer (plastic, ceramic, or
metal) between the new ball and socket.
What are the risks and consequences of having a hip replacement?
Hip replacement complications are rare, although they
can occur. The most prevalent complications are:
- Infection.
- Deep vein thrombosis and pulmonary embolism
- Prosthetic issues, including loosening or dislocation.
- Broken bones around the prosthesis.
- Feeling stiff in your joint.
Results
Full recovery following a hip replacement varies from
person to person, although the majority of individuals are doing well three
months after surgery. Typically, improvements remain for the first year
following surgery.
The replacement hip joint can relieve discomfort and
enhance the hip range of motion. However, you should not anticipate being able
to accomplish all you can before the hip becomes uncomfortable.
High-impact activities, such as jogging or basketball, maybe
too demanding on the artificial joint. However, most people will eventually be
able to participate in lower-impact sports such as swimming, golf, and cycling.
How long will a hip replacement last?
Prosthetic hips used in hip replacements are often
quite durable. Many patients who have a hip replacement maintain the implant for
the remainder of their lives.
Although rare, some patients may require further hip
procedures in the future. Your surgeon will explain what to expect.
Protecting Your Hip Replacement.
You may do a variety of things to safeguard your hip
replacement and extend its life.
- Exercise regularly to maintain hip strength and mobility.
- Take care to prevent falls and accidents. If you break a bone in your leg,
you may need further surgery.
- Inform your dentist about your hip replacement. Consult your orthopedic
surgeon about whether you need to take antibiotics before dental operations.
- Even if your hip replacement appears to be functioning properly, schedule
frequent follow-up tests and X-rays with your orthopedic surgeon regularly.